Wistar Scientists Recognized at International Society for Vaccines Conference
Wistar researchers were recognized for their leadership and contributions to vaccinology recently at the International Society for Vaccines (ISV) annual Congress. The conference, held in October in Seoul, also featured presentations by scientists in Wistar’s Weiner Lab, who shared some of their latest vaccine research.
Jillian Eisenhauer, a 5th year Ph.D. student at The Wistar Institute, was among the early-career scientists recognized at the conference. She said the meeting underscored Wistar’s importance in the field.
“Overall, Wistar’s representation at ISV serves as an indicator of the Institute’s prominent role in vaccinology/immunology, whether through the research we presented, showcasing our strong collaborations, or, as a graduate student, the ability to interact with and to educate the next generation of scientists,” she said.
Highlights of the conference included:
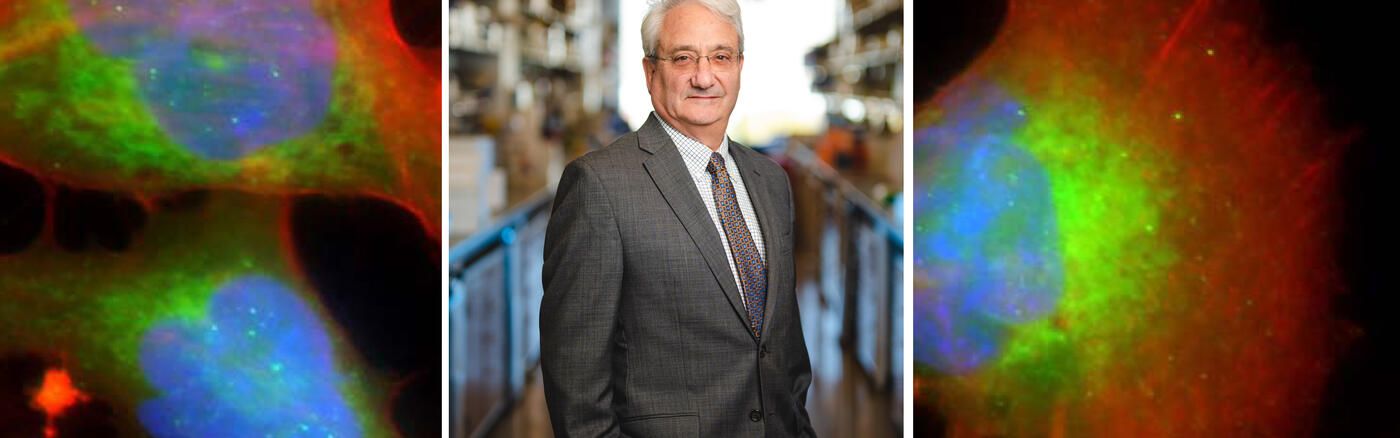
Dr. David Weiner, executive vice president of The Wistar Institute, director of Wistar’s Vaccine & Immunotherapy Center (VIC), and the W.W. Smith Charitable Trust Distinguished Professor in Cancer Research, was re-elected to the board of the International Society for Vaccines, a role in which he will continue to be a leader for early and translational immunotherapy research. He also presented new research on lipid formulated plasmid DNA vaccines and co-chaired a plenary session on therapeutic vaccines against cancer.
Dr. Ebony Gary, a postdoctoral fellow in the Weiner Lab, was selected for the society’s Next Gen Vaccinologist committee, a group of early-career researchers dedicated to enhancing the visibility of Ph.D. students and post-docs in the field of vaccinology. Gary also gave a presentation on new research into mucosal immunity, with a study showing how vaccination using vaccines that encode immune instructions for guiding the immune responses induced at peripheral sites (like the arm) to induce immunity at mucosal surfaces, where many human pathogens, including COVID-19 and H5N1, flu start their infections.
Dr. Ami Patel, an assistant professor in the Vaccine & Immunotherapy Center, presented new influenza research, including a study investigating the use of DNA-encoded monoclonal antibodies for direct prophylaxis against influenza, either as a standalone or in conjunction with vaccines, particularly for at-risk populations.
Ms. Eisenhauer was invited to present in the selected “Bright Sparks” in Vaccinology series for impressive early-career researchers. She was awarded third best overall study in this section for her talk on gene-delivered antibody development as a potential strategy for the treatment or prevention of antimicrobial-resistant infections.
Noting that it was the first presentation of her career, and only the second conference she had attended, Eisenhauer said it was rewarding to be recognized alongside accomplished postdoctoral researchers from around the world. It should be noted she was the only non-Ph.D. selected to present in this section!
“As far as impact, it was extremely encouraging and motivating to receive this award as a 5th year Ph.D. student,” she said.
Gary said she was excited to be contributing to the shared vision of ISV by helping to create opportunities for early-career researchers.
“Being a part of the Next Gen Vaccine committee is wonderful, and I was thrilled to present the work the committee has been doing over the past year to the ISV board,” she said.
She said Wistar was well represented at the international meeting. “All of our talks were well received,” she said. “For VIC members, this meeting is wonderful because it is so specifically focused on all aspects of vaccinology and immune based approaches. Having our abstracts accepted for presentation shows that our research efforts are valued by the vaccine community as a whole.”