The Wistar Institute’s Vaccine & Immunotherapy Center (VIC) has assembled its expertise in infectious disease research, as its scientists are part of a team racing to provide a countermeasure for the ongoing coronavirus outbreak.
A historic leader with a track record of successful vaccines that have saved millions of lives, Wistar is now leveraging synthetic DNA technology to develop a vaccine against the coronavirus.
The laboratory of Dr. David Weiner, Wistar executive vice president, director of the VIC and the W.W. Smith Charitable Trust Professor in Cancer Research, has worked for several decades advancing the technology for generating synthetic DNA vaccines that can be used for global pandemic outbreaks.
In December 2019, Drs. Weiner, Ami Patel, Kar Muthumani, and Dan Kulp at Wistar along with colleagues at Inovio Pharmaceuticals, Inc., Drs. Joseph Kim, Laurent Humeau and Kate Broderick, were paying particular attention to the new outbreak in Wuhan, China, caused by a virus identified as a novel coronavirus. Infections were rapidly expanding in China, and by mid-January they were starting to spill over to other countries. COVID-19, as the infection was eventually named, was not going away. The team decided to work together tackling the outbreak as soon as the opportunity to jump in arose, as they have collaborated to advance vaccines for other outbreak pathogens.
Synthetic DNA would not need the virus itself to build vaccine candidates, as these can be modeled and developed through computer analysis of the viral sequence, using predictions based on prior experience to synthesize a prototype DNA vaccine for rapid testing. The team would use their extensive MERS coronavirus vaccine experience as a model, taking into account unique features displayed by the new coronavirus in the design. In January, as the cases increased, a consortium led by Dr. Yong-Zhen Zhang of the Shanghai Public Health Clinical Center & School of Public Health posted the first viral DNA sequences online.
“This provided the opportunity the team was waiting for,” said Dr. Weiner. Within hours, prototype vaccines were designed and moved to development.
The designed DNA vaccine encodes a tailored sequence as the code for the vaccine. When the vaccine is administered to a recipient, the genetic sequences are then delivered inside the cells and instruct the cells to assemble a new protein shaped like a piece of the virus. Similar to using Lego blocks, a 3-D replica of a viral antigen is built inside the body and teaches the immune system what to look out for and destroy — reproducing what would happen if the person came in contact with the true virus.
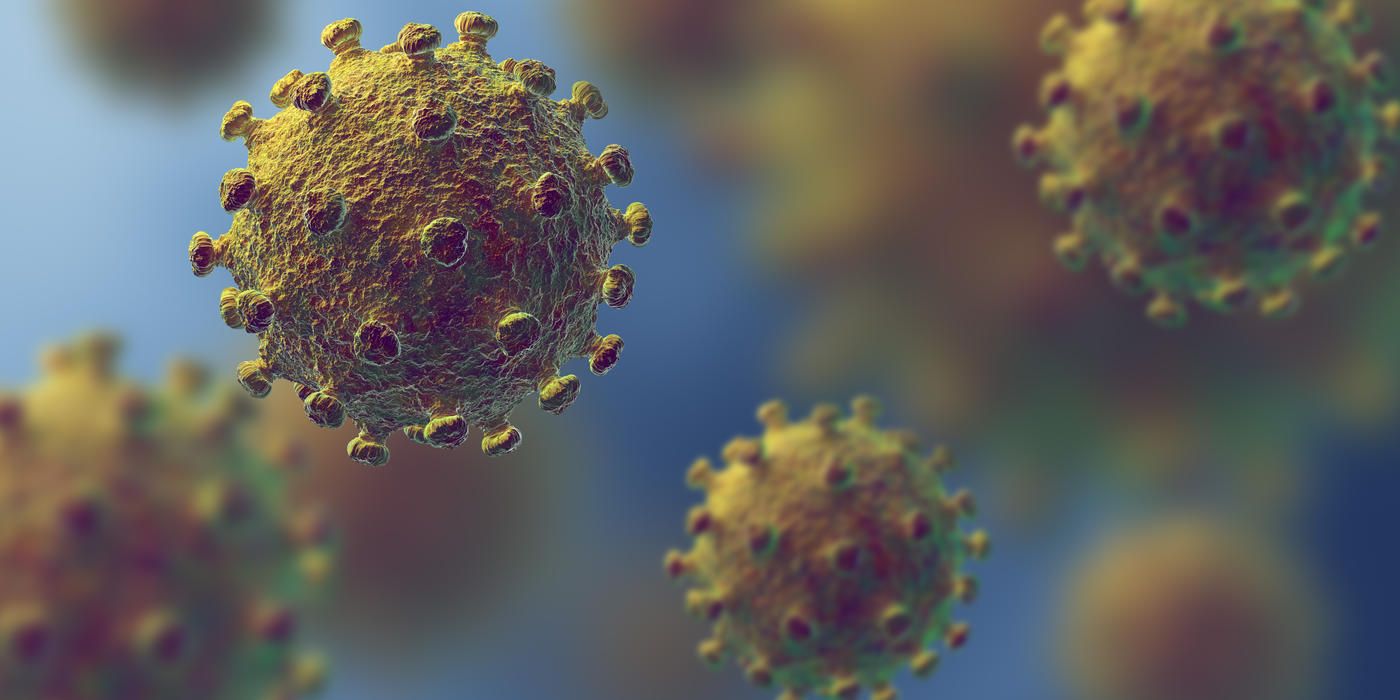
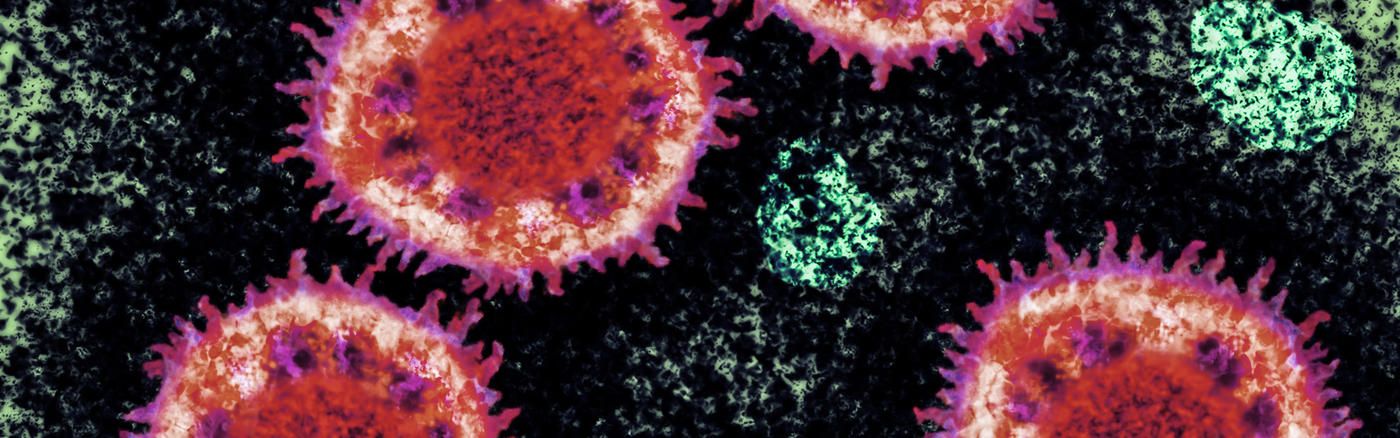
Coronaviruses are large RNA viruses that get their name from the ‘halo’ generated by the spike protein that decorates the surface of these viruses. When a coronavirus is viewed in the laboratory using electron microscopy, the spike proteins appear to form a crown. The new strain of coronavirus has been designated SARS-CoV-2 and is the entity that causes the COVID-19 disease.
SARS-CoV-2 is an emerging pathogen that human populations have not previously experienced although it belongs to the same family as the coronaviruses that caused Severe Acute Respiratory Syndrome (SARS), an outbreak originating in China that the world experienced in the early 2000s, and Middle East Respiratory Syndrome (MERS), an outbreak originating about a decade later in the Middle East that, while controlled, still smolders.
The team has significant experience in developing countermeasures for a coronavirus outbreak. A synthetic DNA MERS vaccine they developed advanced into phase 2 clinical study, having achieved relevant vaccine milestones including protection of laboratory animals from infection, human safety, and immunogenicity.
The new coronavirus vaccine effort by the Weiner team is one of a handful supported by the Coalition for Epidemic Preparedness Innovations (CEPI) for the rapid development of new vaccine approaches to the coronavirus outbreak. CEPI is a global alliance led by Norway along with several other countries with major funding from philanthropic organizations. Assembled just more than three years ago to fast-track translational vaccine approaches for emerging pandemics, the organization has been comparing vaccine technologies that could be utilized rapidly in an outbreak situation with the foresight of stemming worldwide epidemics using scientific innovations through new technology.
That preparation is being put to the test in support of developing a vaccine response for COVID-19. In January, CEPI started to discuss funding a program for clinical vaccine development with the team. On January 23, at the World Economic Forum in Davos, CEPI announced its support for three teams based on their technologies and accomplishments showing their vaccines can be rapidly created, tested, generate consistent immunity, and can be advanced in a conceptually safe fashion to clinical trials.
Each team funded by CEPI is comprised of industry partners and academic vaccine teams that work together to move the novel candidates through early development and into clinical study and then, if applicable, advance them to efficacy trials. This approach combines the research speed of academic investigators with the focused development and clinical production and regulatory strengths of industry leaders who are at the forefront of their technologies.
The Initial teams were:
- GlaxoSmithKline (GSK) in partnership with the University of Queensland, Australia, for a recombinant protein and adjuvant approach.
- Moderna Therapeutics, Inc., in partnership with the National Institute of Allergy and Infectious Diseases (NIAID) Vaccine Research Center for a mRNA approach; and
- Inovio in partnership with The Wistar Institute’s VIC team.
Five additional teams have recently been added by CEPI.
“It’s a very unique situation — it’s the first time we’re seeing a global vaccine coordinated response like this, thanks to the speed with which CEPI acted and funded the initial teams,” said Weiner. “We are honored to be able to contribute to this important effort under the advanced DNA vaccine technology program of Inovio for COVID-19.”
The team reported immune responses to the new synthetic DNA vaccine that were induced in several animal model species after a single immunization — the first program to do so.
CEPI’s stated initial goal was to speed advancement of the new coronavirus vaccines to phase 1 trials in four months or less. The CEPI program has made a significant difference already in mobilizing the vaccine community to advance products for COVID-19. This week, Moderna announced that they have opened their phase 1 clinical trial. Inovio announced that a phase 1 study of the synthetic DNA vaccine is preparing to open in April.
As of March 23, just 3.5 months into this outbreak, there are approximately 372,000 reported infections with more than 16,300 deaths spread over 168 countries. In the U.S., there are over 41,000 cases which have resulted in 573 fatalities. New York has more than 12,000 cases*.
“The Wistar Institute’s VIC works to provide new immune approaches and understanding to impact important human disease. We need countermeasures for the COVID-19 pandemic,” said Weiner. “All of us are in this together and the more tools in the toolbox, the better equipped we are to possibly protect our vulnerable populations and our first-line defenders. Rapidly advancing these tools is only the first step in this process, but it’s an important one.”
* Source: Center for Systems Science and Engineering at Johns Hopkins University