PHILADELPHIA — (Feb. 1, 2022) — The first generation of COVID-19 vaccines have been highly effective, but also have limitations: their efficacy can wane without a booster shot, and they may be less effective against some variants. Now scientists at The Wistar Institute have developed a more targeted vaccine that, in animal studies, shows stronger, broader, and more durable protection in a single, low dose.
The vaccine combines three technologies – immune focusing, self-assembling nanoparticles, and DNA delivery – into a single platform for the first time. In addition to its other advantages, the vaccine could be stored at room temperature, making it potentially easier to transport to remote or developing locations.
“This is among the first next-generation vaccines that will have more advanced features and broader protection,” said Daniel Kulp, Ph.D., associate professor in the Vaccine & Immunotherapy Center at The Wistar Institute and corresponding author of the study.
The paper, “Nucleic acid delivery of immune-focused SARS-CoV-2 nanoparticles drive rapid and potent immunogenicity capable of single-dose protection,” was published in the journal Cell Reports.
Existing vaccines include an unmodifided receptor binding domain of SARS-CoV-2 spike protein. The new vaccine includes a rationally engineered receptor binding domain using computational and structure-based design methodologies. The engineered receptor binding domain blocks ‘immune distracting’ sites and can therefore elicit stronger levels of protective, neutralizing antibodies.
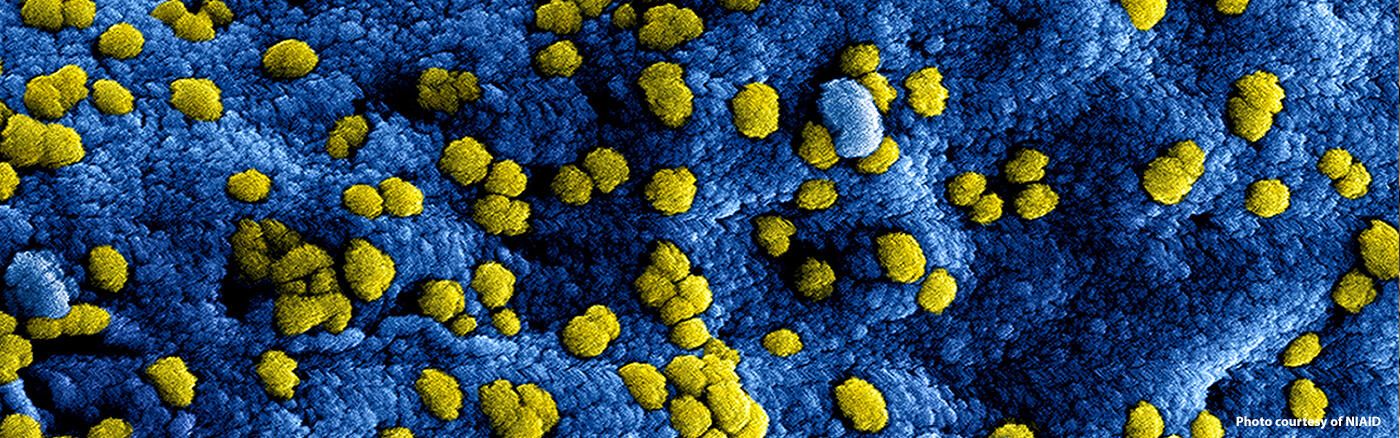
Researchers then used naturally self-assembling proteins to form nanoparticles which display these highly engineered immunogens. By arranging themselves into structures that resemble an actual virus, the nanoparticles are more easily recognized by the immune system and transported to the germinal centers, where they activate B cells which produce protective antibodies.
Using nucleic acid vaccine delivery technology similar to mRNA, the nanoparticle vaccine is encoded in DNA and delivered into cells thereby giving genetic instructions for the body to build the immunogen internally. This is an advance over traditional vaccines that must be manufactured in specialized factories through complex vaccine production processes. In contrast to other vaccines, Dr. Kulp noted that one advantage of the DNA platform is that it doesn’t require refrigeration and it can also be quickly reformulated to target new variants.
In animal models, researchers found that the DNA delivered immune-focused nanoparticle vaccine produced much higher levels of neutralizing antibodies than the vaccine that wasn’t immune-focused.
“A difficulty with current vaccines is that neutralizing antibodies decline over time,” Kulp said. The nanoparticle vaccine produced durable responses after a single immunization out to six months in mice, unlike what we are seeing with current SARS-CoV-2 vaccines in people.
The ultimate test for SARS-CoV-2 vaccine candidates is protection from death in SARS-CoV-2 challenge experiments. The researchers found that in a lethal challenge model 100% of mice who received the immune-focused nanoparticle vaccine were protected from death with a single low dose. Most mice who received the standard, non-immune focused vaccine died within 10 days of challenge.
The vaccine assessment was conducted in both wild-type mice and mice that were genetically engineered to mimic human immune systems, he noted.
Even without being updated, the immune-focused vaccine showed a comparable level of antibody production to Delta, and other variants, Kulp said. That’s partly because of the immune focusing approach itself, he noted; in blocking parts of the receptive binding domain for the purpose of inhibiting non-neutralizing antibodies, it also blocks many of the areas affected by spike protein mutations. Studies on the Omicron variant are underway.
Researchers are seeking funding to begin human trials of the vaccine.
Co-author David B. Weiner, Ph.D., executive vice president, director of the Vaccine & Immunotherapy Center and the W.W. Smith Charitable Trust Professor in Cancer Research, at The Wistar Institute, said the vaccine could provide a needed step forward to improve protection against COVID-19.
“Current vaccine effects on reducing transmission of SARS-CoV-2 variants of concern including Delta and Omicron could be improved for their breadth of protection as well as their immune potency,” Weiner said. “This study demonstrates that using a nucleic acid approach combined with in vivo structural assembly of a glycan immune-focused nanoparticle drives single protection and neutralization against diverse variants of concern in a dose-sparing formulation. Additional studies of this vaccine approach for SARS-CoV-2 appear timely and important.”
Co-authors: Kylie M. Konrath, Kevin Liaw, Yuanhan Wu, Xizhou Zhu, Susanne N. Walker, Ziyang Xu, Neethu Chokkalingam, Nicholas J. Tursi, Mansi Purwar, Emma Reuschel, Drew Frase, Benjamin Fry, and Ami Patel from Wistar; Katherine Schultheis, Igor Maricic, Viviane M. Andrade, Kate E. Broderick, Laurent M.P.F. Humeau, and Trevor R.F. Smith from Inovio Pharmaceuticals; Himanshi Chawla and Max Crispin from the University of Southhampton; Jianqiu Du and Alan Moore from Indiana University; Jared Adolf-Bryfogle and Jesper Pallesen from the Institute for Protein Innovation; Matthew Sullivan from the University of Pennsylvania; and Christel Iffland from Ligand Pharmaceuticals.
Work supported by: Wistar Coronavirus Discovery Fund, CURE/PA Department of Health grant SAP# 4100083104, COVID/PA Department of Human Services grant SAP# 4100089371, NIH/NIAID CIVICs grant 75N93019C00051, Wistar SRA 16-4 / Inovio Pharmaceuticals, Indiana University.
Publication information: Nucleic acid delivery of immune-focused SARS-CoV-2 nanoparticles drive rapid and potent immunogenicity capable of single-dose protection, Cell Reports, 2022.