A Wistar Journey Through the Past, Present, and Future of Immunization Work
Vaccines are a crucial public health tool in its’ arsenal against diseases. Resurgences of diseases long thought eradicated are popping up decades later in sewage waters here and abroad, and we’ve witnessed what the impact of war has on countries whose health systems have crumbled under the ravages of war—we are not as far removed as we’d like to be from diseases once prevented by vaccines. With more than half a century of basic research for vaccine development, The Wistar Institute plays an integral role in immunization around the globe.
Rubella, rabies, and rotavirus. Wistar scientists developed vaccines for these diseases that are used in immunization programs worldwide. The rubella vaccine by Wistar scientists effectively ended the pandemic in the United States, as declared by the CDC in 2005. Two rabies vaccinations developed from the Institute addresses the disease in both animals and humans. In 2006, Wistar and collaborators created a rotavirus vaccine which became part of the regular immunization schedule for U.S. babies and is used or approved in over 45 countries. And we’re just getting started.
“Immunization is possibly one of the most impactful medical interventions ever developed. Millions of lives are saved each year by vaccination, and we live healthier and longer lives due to vaccines.” states David Weiner, Ph.D., Executive Vice President, Director of Wistar’s Vaccine & Immunotherapy Center, and W.W. Smith Charitable Trust Professor in Cancer Research, in the Immunology, Microenvironment & Metastasis Program at Wistar’s Ellen and Ronald Caplan Cancer Center.
This National Immunization Awareness Month, we have shared a few snapshots of current vaccine development projects at the Institute as well as what these researchers’ hopes are for the future of immunization.
Tackling Both Infectious Disease and Cancer with Immunization
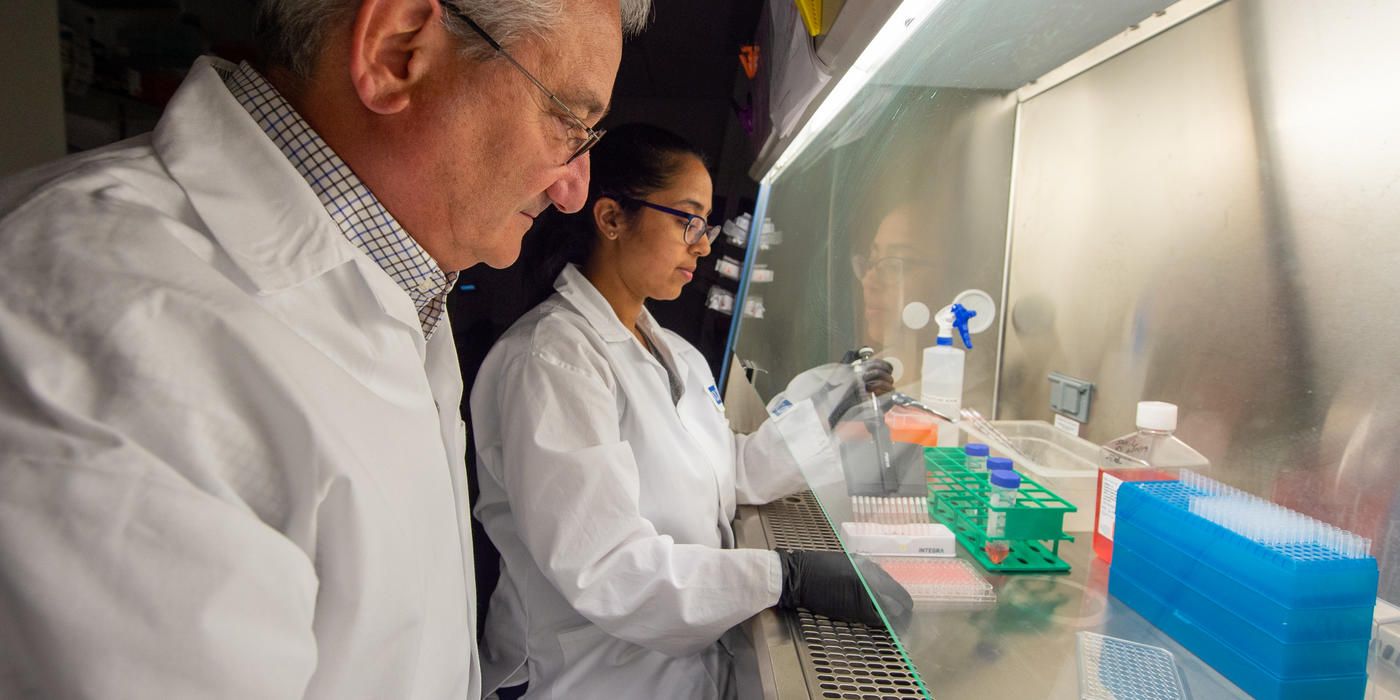
Dr. Weiner’s research takes on both infectious disease and cancer. His work encompasses developing new ways to build and deliver synthetic nucleic acid vaccines – particularly advancing a new approach that drives self-assembly of an antigen into a more potent vaccine inside a vaccinated person. This approach gives the body the genetic information to become the factory to create the vaccine. Furthermore, his lab is developing new types of cancer therapeutic vaccines with the goals of creating strong anti-cancer immunity and eradicating cancer cells.
Weiner’s collaborations with public and private institutions is centered around novel immunization technology developed from his lab called DNA-encoded monoclonal antibodies (DMAbs) against diseases such as COVID-19, Zika, and Ebola.
Regarding the future, he shares, “Together with our collaborators, we hope to move new prototype HIV vaccines into human clinical trials later this year, and continue to advance vaccines for emerging pathogens, as well as cancer immunotherapies.”
Developing DNA Vaccines
Ami Patel, Ph.D., Caspar Wistar Fellow in the Vaccine and Immunotherapy Center, focuses her scientific efforts on DNA vaccines which have potential to be more stable and economical over traditional vaccine production. “We are trying to understand how different vaccines work in the body. How do vaccines generate different types of immune responses and can we use this to understand protection against infectious diseases. We are using this information to help develop the next generation of potential vaccines.” she says.
Patel emphasizes the importance of vaccines for young children and adults by calling back to various infectious diseases like polio that are no longer very common because of immunization. “Vaccines help protect us against serious disease. Some of us remember the discomfort of chicken pox as children. There is now a vaccine.”
While she calls the COVID-19 pandemic “devastating to global health”, Patel also recognizes the pandemic’s challenges proved fertile ground for an extraordinary collaborative time for biomedical scientists. “My hope is for vaccine researchers across different disciplines to continue to work together to help us understand different infectious diseases and develop better vaccines.”
Zooming in on a Nanoscale
In collaboration with Weiner, Daniel Kulp, Ph.D., associate professor in the Vaccine and Immunotherapy Center, has embraced nanotechnology in his vaccine research. “We are developing rationally engineered nanoparticle vaccines that can elicit extremely broad coronavirus immunity providing a proof-of-concept that a pan-coronavirus vaccine is possible,” Kulp elaborates.
While the Kulp laboratory is developing several promising vaccines, he emphasizes that his goal is to assess these candidates in humans. He says, “We are working to reduce barriers for launching small experimental medicine clinical trials allowing for broader evaluation of our best vaccine concepts. Through this type of work, I have high hopes that our generation can claim credit for the eradication of SARS-CoV-2.”
Kulp expresses that “Vaccines are one of the single most effective medical technologies humans have developed saving hundreds of millions of lives. Vaccines do not work without immunizations. This message is incredibly important.”