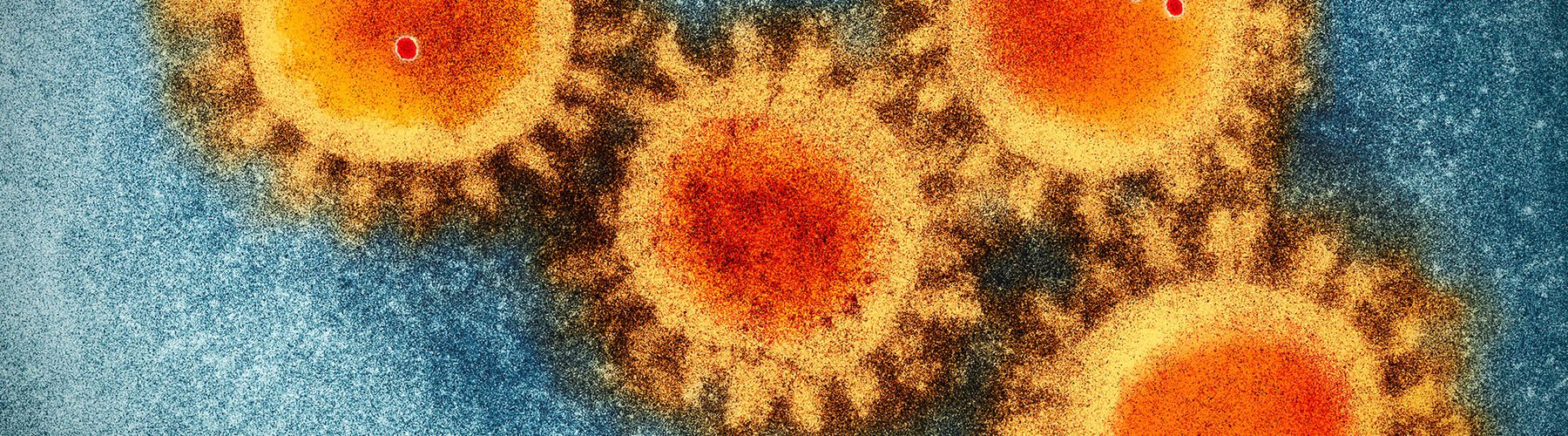
Dr. Luis Montaner is a transformative leader in HIV research. Throughout his tenure at Wistar, his discoveries to find an HIV cure have elevated both the prestige and scientific prowess of the Institute while most importantly, helped inform the treatments for people around the globe suffering from HIV.
Montaner has spent the last 26 years at The Wistar Institute researching HIV infection and how to boost the immune system to fight the disease. With the goal of advancing treatment strategies toward HIV eradication, his research combines virology and immunology to study the mechanisms of HIV virus infection. Montaner is also involved in overseeing patient enrollment into innovative clinical trials through advocacy partners such as Philadelphia FIGHT, and this summer, he and his partners were awarded a $29.15 million Martin Delaney Collaboratories for HIV Cure Research award to the BEAT-HIV Martin Delaney Collaboratory to advance combination immunotherapy research towards a cure for HIV. This funding extends a grant originally awarded in 2016 based on research progress to date.
Dr. Luis Montaner joined Wistar in 1995 as an assistant professor and was promoted to professor in 2007. He holds many positions at Wistar including vice president, Scientific Operations; Hebert Kean, M.D., Family Professor; associate director for Shared Resources, The Wistar Institute Cancer Center; and director, HIV-1 Immunopathogenesis Laboratory and leader, HIV Research Program. Since his arrival, Luis has been a proponent of the power of scientific collaboration. He believes that by joining intellectual and resource strengths with partners, he can advance research faster and achieve better outcomes. As illustrated in the map, the Montaner lab collaborative studies extend from Philadelphia across the United States and Puerto Rico to Mexico, Europe, South America, Southern Africa, and Asia.
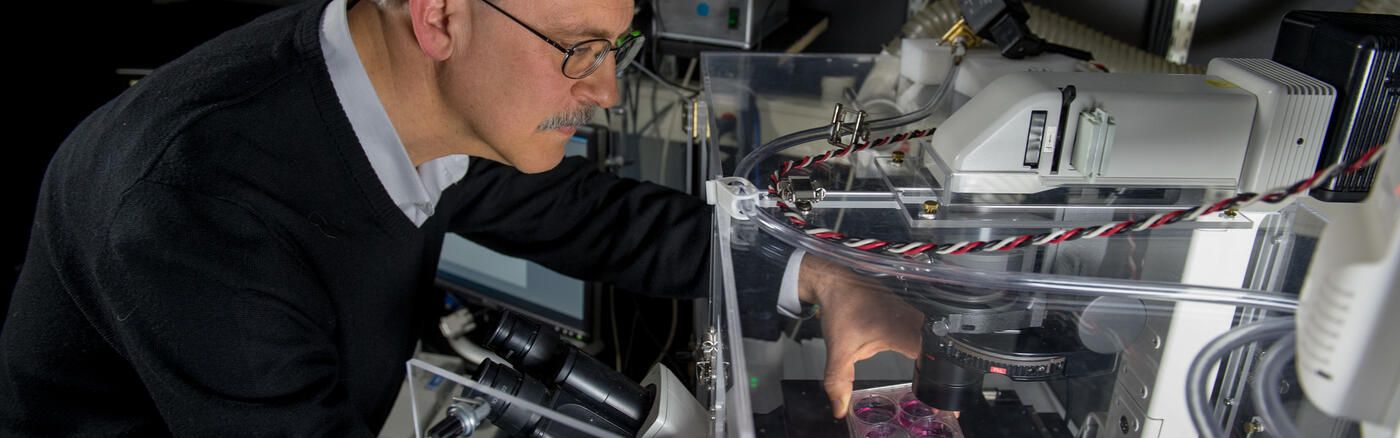
His work relies on laboratory models of viral infection, such as animal models, together with clinical cohort studies, to provide a clinic-to-bench research program. This approach informs new strategies to combat HIV that may also change how we think about prevention and treatment of other infectious diseases and cancer.
“Research moves faster and with greater impact when you bring together several experts with different knowledge and areas of discovery,” said Dr. Montaner. “Just like an orchestra conductor can draw different sounds to support the execution of a symphony, the ability to draw from basic researchers, animal model experts, clinicians, industry experts, international advisors, and community members under a common shared effort helps us accelerate progress towards an HIV cure.”
Nothing exemplifies the power of collaboration more than the incredible progress the HIV research field has enabled over the last forty years in diagnosing, treating, and preventing HIV. Even recently, from 2010 to 2017, the rate of HIV-related deaths among people 13 years and older in the United States fell by nearly half according to a study from the Center for Disease Control and Prevention.
Much has been accomplished in the HIV research field, however there is still so much more to do, including the continued pursuit of a successful HIV vaccine and ultimately a cure for HIV. In this pursuit for a cure, Dr. Montaner currently leads one of the largest coalitions of NIH-funded, HIV cure-directed research under the BEAT-HIV Delaney Collaboratory. This enormous consortium brings together more than 70 top HIV researchers from academic research institutions around the world working with government, nonprofit organizations, and industry partners to test combinations of several novel immunotherapies under new preclinical research and clinical trials. The common goal of the Collaboratory is to achieve an accessible and safe strategy that can either sustain control of HIV without the continued use of current therapies and/or eradicate HIV.
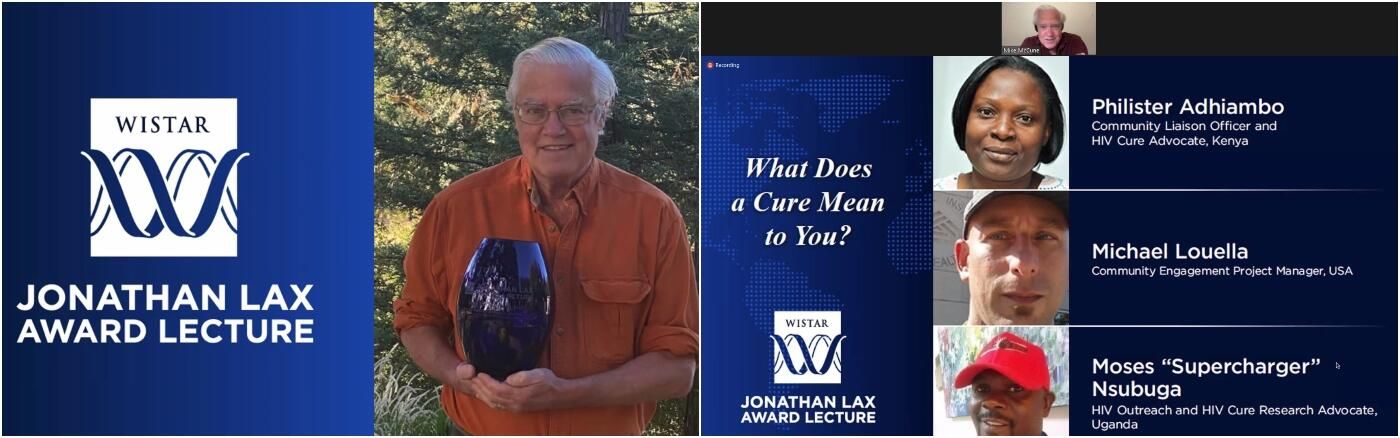
While global collaborations are important, Luis has always been a huge proponent of the power of local collaborations. Within Philadelphia, his lab has a long-standing partnership with Philadelphia FIGHT, a comprehensive health services organization providing primary care, consumer education, research and advocacy for people living with HIV/AIDS and those at high risk. Representing an academic-community partnership that is unique in HIV research, Philadelphia FIGHT and the University of Pennsylvania along with the Robert I. Jacobs Fund of The Philadelphia Foundation, developed the HIV-1 Patient Partnership Program to provide clinical material for basic research and to sponsor the Jonathan Lax Memorial Lecture. Research with clinical material obtained from this Program is focused on mechanisms of AIDS immunopathology. This collaborative link between Montaner’s research team and more than 5,000 people living with HIV/AIDS in the Philadelphia region has led to the largest HIV Cure clinical trial to date — the BEAT-HIV Study. Their partnership with Philadelphia FIGHT strives to develop trusted relationships and maintain meaningful, bi-directional lines of communication between scientists and communities most affected by HIV. HIV Social Science has been a recent addition to the Montaner lab program to enhance both their preclinical and community engagement efforts.
Opportunity for progress is unique and unparalleled at present but so is Wistar’s collective responsibility to deliver.