Wistar Scientists Identify Pro-aging ‘Sugar Signature’ in the Blood of People Living with HIV

-
CONTACT:
-
Darien Sutton
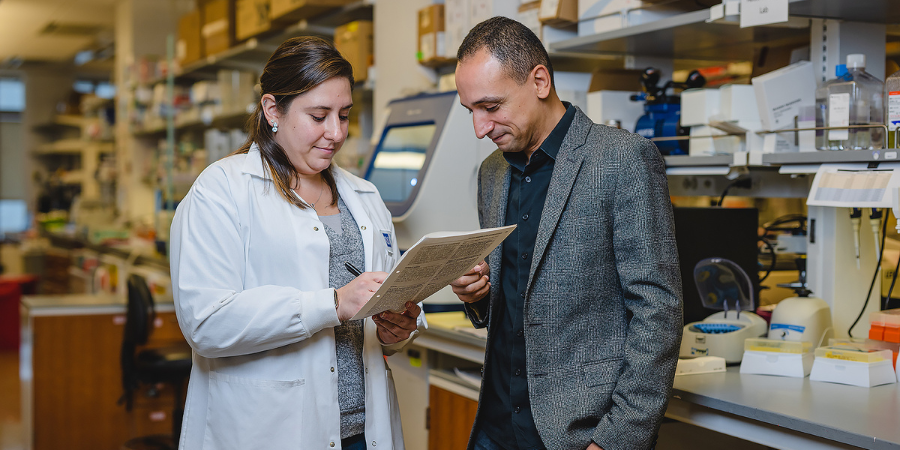
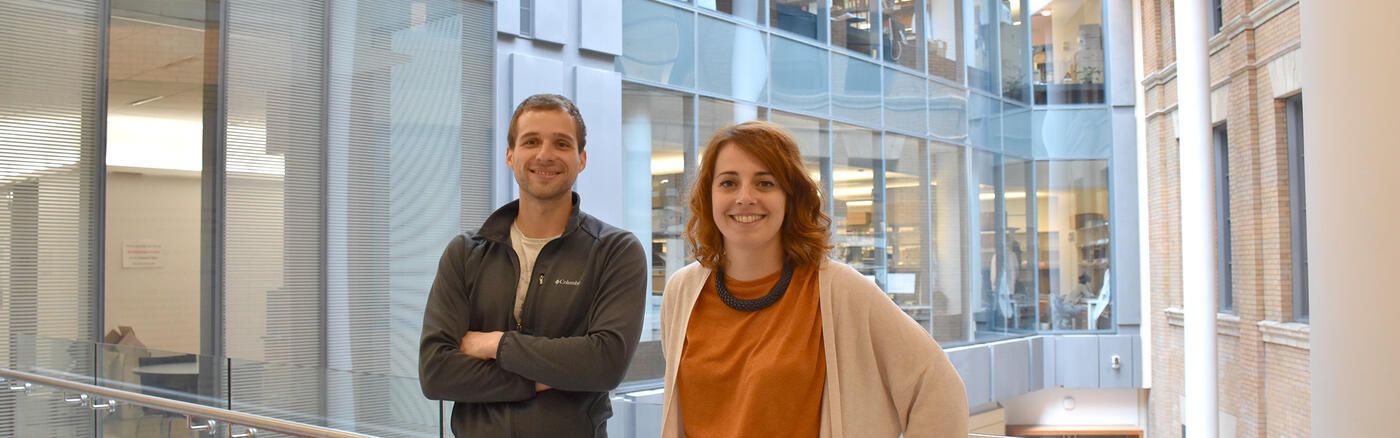
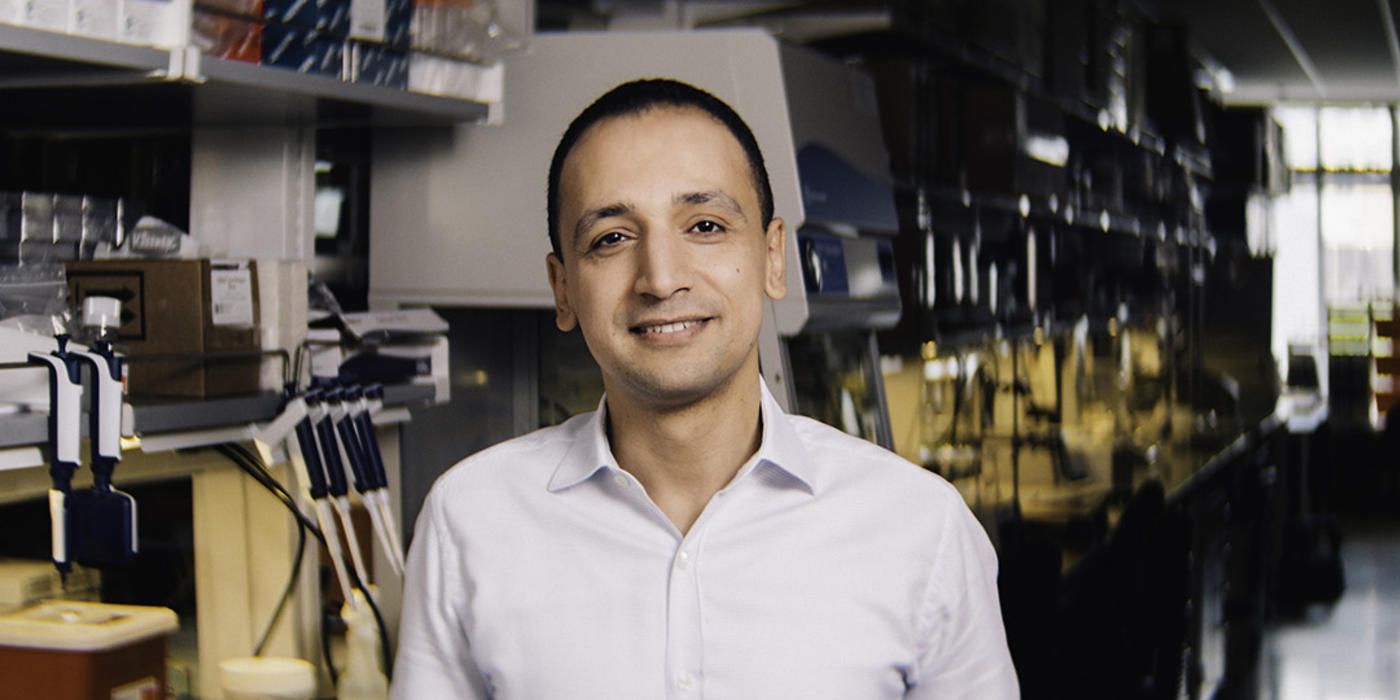
PHILADELPHIA — (April 10, 2024) — The Wistar Institute’s associate professor Mohamed Abdel-Mohsen, Ph.D., along with his team and collaborators, has identified sugar abnormalities in the blood that may promote biological aging and inflammation in people living with HIV (PLWH). The findings, taken from a large data study comprising more than 1200 participants, are detailed in the new paper, “Immunoglobulin G N-glycan Markers of Accelerated Biological Aging During Chronic HIV Infection,” published in the journal Nature Communications.
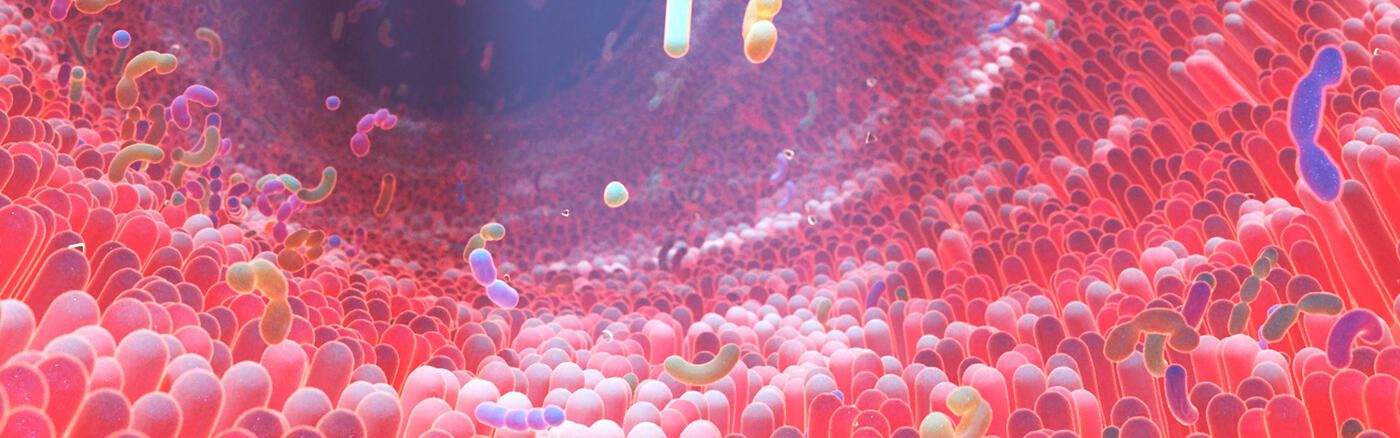
Despite advances in HIV treatment, notably the success of antiretroviral therapy (ART) in suppressing the virus to undetectable levels, HIV remains incurable, with the virus persisting in a dormant state within the body. This chronic presence is linked to long-term health issues, including persistent inflammation and a higher prevalence of aging-related diseases such as cancer and neurocognitive disorders. These conditions tend to occur more frequently and at an earlier age in PLWH compared to the general population.
Abdel-Mohsen seeks to understand how chronic viral infection causes this accelerated biological aging, which refers to the body aging faster than one’s chronological years would typically indicate. By understanding the molecular mechanisms behind accelerated biological aging in people living with chronic viral infections, scientists can begin to formulate strategies to mitigate the negative effects.
While many factors in the body can contribute to accelerated biological aging, researchers focused on a novel factor: abnormalities of the human glycome — the totality of the various sugar structures circulating throughout the body. Previous studies have established a connection between aging and shifts in the glycan composition of immunoglobulins (IgGs), which are critical for immune regulation. As people age, their IgGs lose anti-inflammatory properties and gain pro-inflammatory characteristics.
Abdel-Mohsen’s research investigates whether living with a chronic viral infection, such as HIV infection, exacerbates these changes, leading to premature aging and related diseases. By comparing glycan profiles in more than 1200 individuals, both with and without HIV, the team discovered that PLWH exhibit elevated levels of inflammatory and pro-aging IgG glycan signatures. In a remarkable step forward, the team developed a machine-learning model that uses these glycan signatures to estimate the biological age of PLWH and assess the rate of aging acceleration. This glycan signature also has the potential to predict the onset of comorbid conditions in PLWH, such as cancer, years in advance.
To confirm that these glycan-associated disruptions were causal rather than merely correlative, the research team engineered HIV-specific antibodies designed to exhibit the same kind of aberrant IgG glycan modifications observed in PLWH. Testing these glycoengineered antibodies in vitro confirmed that the modified antibodies were less effective at mounting an immune response than their unmodified counterparts, suggesting that these sugar abnormalities might directly contribute to the worse clinical outcomes observed. Importantly, when they designed these antibodies to have glycans similar to those found in biologically younger individuals, these antibodies demonstrated a remarkable ability to enhance the immune system’s ability to fight virus-infected cells.
“Utilizing glycan signatures to predict early onset of diseases in people living with HIV marks a pivotal shift towards proactive healthcare,” said Abdel-Mohsen. “This could significantly alter clinical outcomes, allowing for timely interventions and personalized treatment plans. The impact on treatment and management in the HIV community could be revolutionary. Beyond biomarkers, antibodies glycoengineered to mimic biologically younger glycans offer a new therapeutic avenue. This method could enhance immune responses, paving the way for innovative treatments.”
Co-authors: Leila B Giron, Qin Liu, Opeyemi S Adeniji, Xiangfan Yin, Toshitha Kannan, Jianyi Ding, David Y. Lu, Joao L. L. C. Azevedo, Andrew Kossenkov, and Mohamed Abdel-Mohsen of The Wistar Institute; David Y. Lu of Cornell University; Susan Langan, Jinbing Zhang, Sabina Haberlen, Stephen Gange, Wendy S. Post, and Todd T. Brown of Johns Hopkins University; Shuk Hang Li and Ian Frank of the University of Pennsylvania Perelman School of Medicine; Sergei Shalygin and Parastoo Azadi of University of Georgia; David B Hanna of Albert Einstein College of Medicine; Igho Ofotokun of Emory University School of Medicine; Jason Lazar of SUNY Downstate Health Sciences University; Margaret A. Fischl of University of Miami; Bernard Macatangay and Charles Rinaldo of University of Pittsburgh; Adaora A. Adimora of University of North Carolina, Chapel Hill; Beth D. Jamieson of University of California, Los Angeles; Daniel Merenstein of Georgetown University Medical Center; Nadia R. Roan of Gladstone Institutes and University of California, San Francisco; Phyllis C. Tien of University ofCalifornia, San Francisco; Olaf Kutsch of University of Alabama at Birmingham; Steven M. Wolinsky of Northwestern University; Mallory D. Witt of Lundquist Institute of Biomedical Research at Harbor-UCLA Medical Center; and Alan Landay of Rush University.
Work supported by: This work is mainly supported by the NIH R01AG062383 and the NCI supplement to the Wistar Institute Cancer Center (P30 CA010815) to M.A-M. M.A-M is also funded by the NIH grants, R01AI165079, R01NS117458, R01DK123733, Penn Center for AIDS Research (P30 AI 045008), and the NIH-funded BEAT-HIV Martin Delaney Collaboratory to cure HIV-1 infection (1UM1Al126620). Mass spectrometry-based glycomic analyses was partially supported by NIH R24GM137782 and GlycoMIP, a National Science Foundation Materials Innovation Platform funded through Cooperative Agreement DMR-1933525. We would like to thank Drs. Michel Nussenzweig, Costin Tomescu, and Luis J. Montaner for providing the wild-type 10-1074 for the glycoengineering experiments and Dr. Daniel Kulp for providing HIV-1 Env trimer, BG505. Data in this manuscript were collected by the MACS/WIHS Combined Cohort Study (MWCCS). The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH). MWCCS (Principal Investigators): Atlanta CRS (Ighovwerha Ofotokun, Anandi Sheth, and Gina Wingood), U01-HL146241; Baltimore CRS (Todd Brown and Joseph Margolick), U01-HL146201; Bronx CRS (Kathryn Anastos, David Hanna, and Anjali Sharma), U01-HL146204; Brooklyn CRS (Deborah Gustafson and Tracey Wilson), U01-HL146202; Data Analysis and Coordination Center (Gypsyamber D’Souza, Stephen Gange and Elizabeth Topper), U01-HL146193; Chicago-Cook County CRS (Mardge Cohen and Audrey French), U01-HL146245; Chicago-Northwestern CRS (Steven Wolinsky, Frank Palella, and Valentina Stosor), U01-HL146240; Northern California CRS (Bradley Aouizerat, Jennifer Price, and Phyllis Tien), U01-HL146242; Los Angeles CRS (Roger Detels and Matthew Mimiaga), U01-HL146333; Metropolitan Washington CRS (Seble Kassaye and Daniel Merenstein), U01-HL146205; Miami CRS (Maria Alcaide, Margaret Fischl, and Deborah Jones), U01-HL146203; Pittsburgh CRS (Jeremy Martinson and Charles Rinaldo), U01-HL146208; UAB-MS CRS (Mirjam-Colette Kempf, Jodie Dionne-Odom, Deborah Konkle-Parker, and James B. Brock), U01-HL146192; UNC CRS (Adaora Adimora and Michelle Floris- Moore), U01-HL146194. The MWCCS is funded primarily by the National Heart, Lung, and Blood Institute (NHLBI), with additional co-funding from the Eunice Kennedy Shriver National Institute Of Child Health & Human Development (NICHD), National Institute On Aging (NIA), National Institute Of Dental & Craniofacial Research (NIDCR), National Institute Of Allergy And Infectious Diseases (NIAID), National Institute Of Neurological Disorders And Stroke (NINDS), National Institute Of Mental Health (NIMH), National Institute On Drug Abuse (NIDA), National Institute Of Nursing Research (NINR), National Cancer Institute (NCI), National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute on Deafness and Other Communication Disorders (NIDCD), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute on Minority Health and Health Disparities (NIMHD), and in coordination and alignment with the research priorities of the National Institutes of Health, Office of AIDS Research (OAR). MWCCS data collection is also supported by UL1-TR000004 (UCSF CTSA), UL1-TR003098 (JHU ICTR), UL1TR001881 (UCLA CTSI), P30-AI-050409 (Atlanta CFAR), P30-AI-073961 (Miami CFAR), P30 AI-050410 (UNC CFAR), P30-AI-027767 (UAB CFAR), P30-MH-116867 (Miami CHARM), UL1 TR001409 (DC CTSA), KL2-TR001432 (DC CTSA), and TL1-TR001431 (DC CTSA). The MACS CVD2 study is funded by National Heart Lung and Blood Institute (NHLBI), R01 HL095129-01 (Wendy Post). The authors gratefully acknowledge the contributions of study participants and dedication of the staff at MWCCS sites.
Publication information: “Immunoglobulin G N-glycan 1 Markers of Accelerated Biological Aging During Chronic HIV Infection,” from Nature Communications.
For a printer-friendly version of this release, please click here.
ABOUT THE WISTAR INSTITUTE:
The Wistar Institute is the nation’s first independent nonprofit institution devoted exclusively to foundational biomedical research and training. Since 1972, the Institute has held National Cancer Institute (NCI)-designated Cancer Center status. Through a culture and commitment to biomedical collaboration and innovation, Wistar science leads to breakthrough early-stage discoveries and life science sector start-ups. Wistar scientists are dedicated to solving some of the world’s most challenging problems in the field of cancer and immunology, advancing human health through early-stage discovery and training the next generation of biomedical researchers. wistar.org.