

Wistar News
Our Scientists
Through a culture and commitment to biomedical collaboration and innovation, Wistar science leads to breakthrough early-stage discoveries that improve human health.
Cancer
Wistar is an NCI-designated Cancer Center in basic research, and in 2022 the newly renamed Ellen and Ronald Caplan Cancer Center was among the first to earn the prestigious Cancer Center Support Grant Merit Extension from the NCI.

Vaccine &
Immunotherapy
The Vaccine & Immunotherapy Center focuses the Institute’s strengths in immunology, virology and immuno-oncology disciplines to improve public health around the globe.
Education & Training
The Hubert J.P. Schoemaker Education and Training Center brings all Wistar education and training programs under a single umbrella to make lasting global impact in biomedical research.
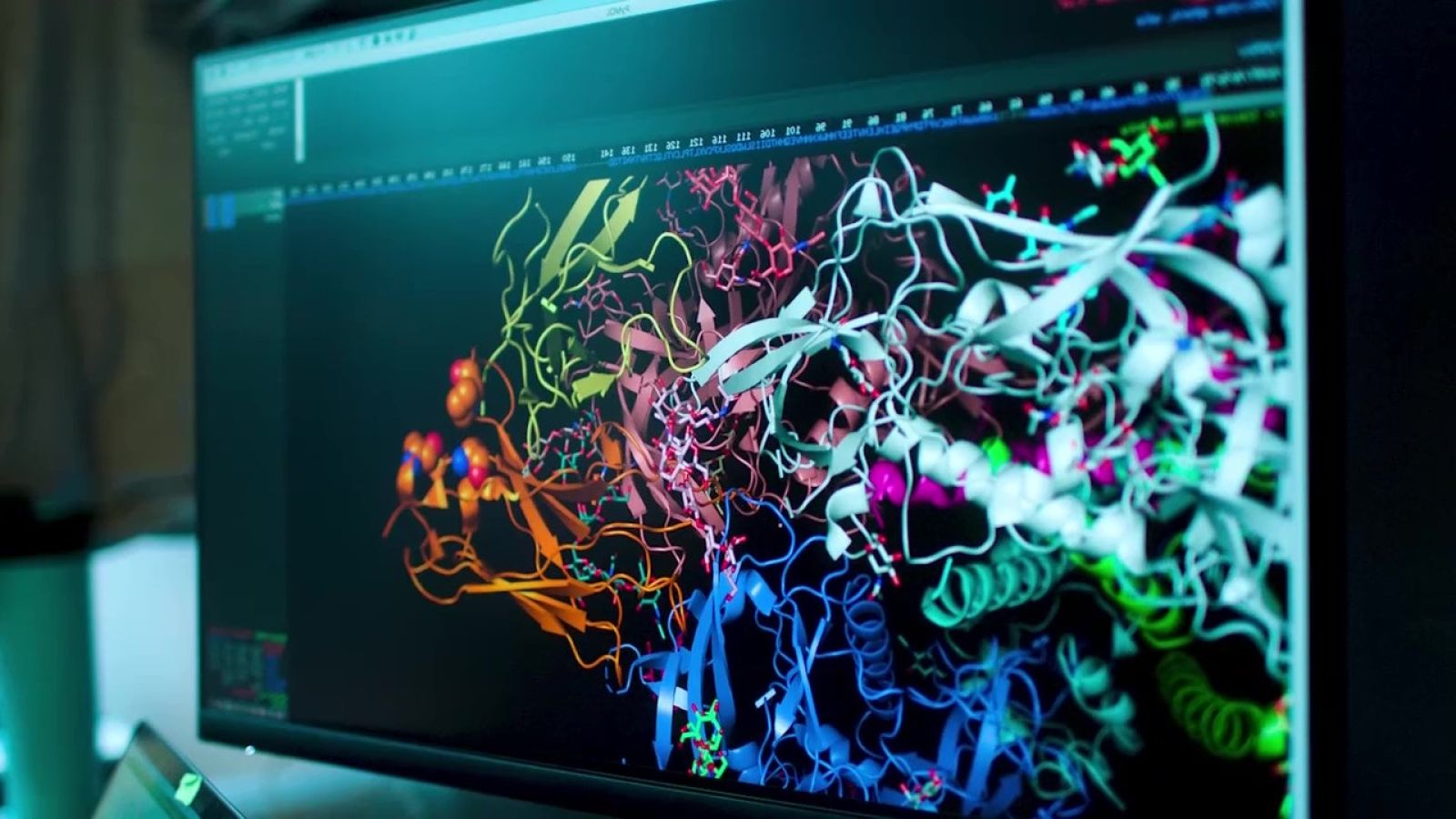
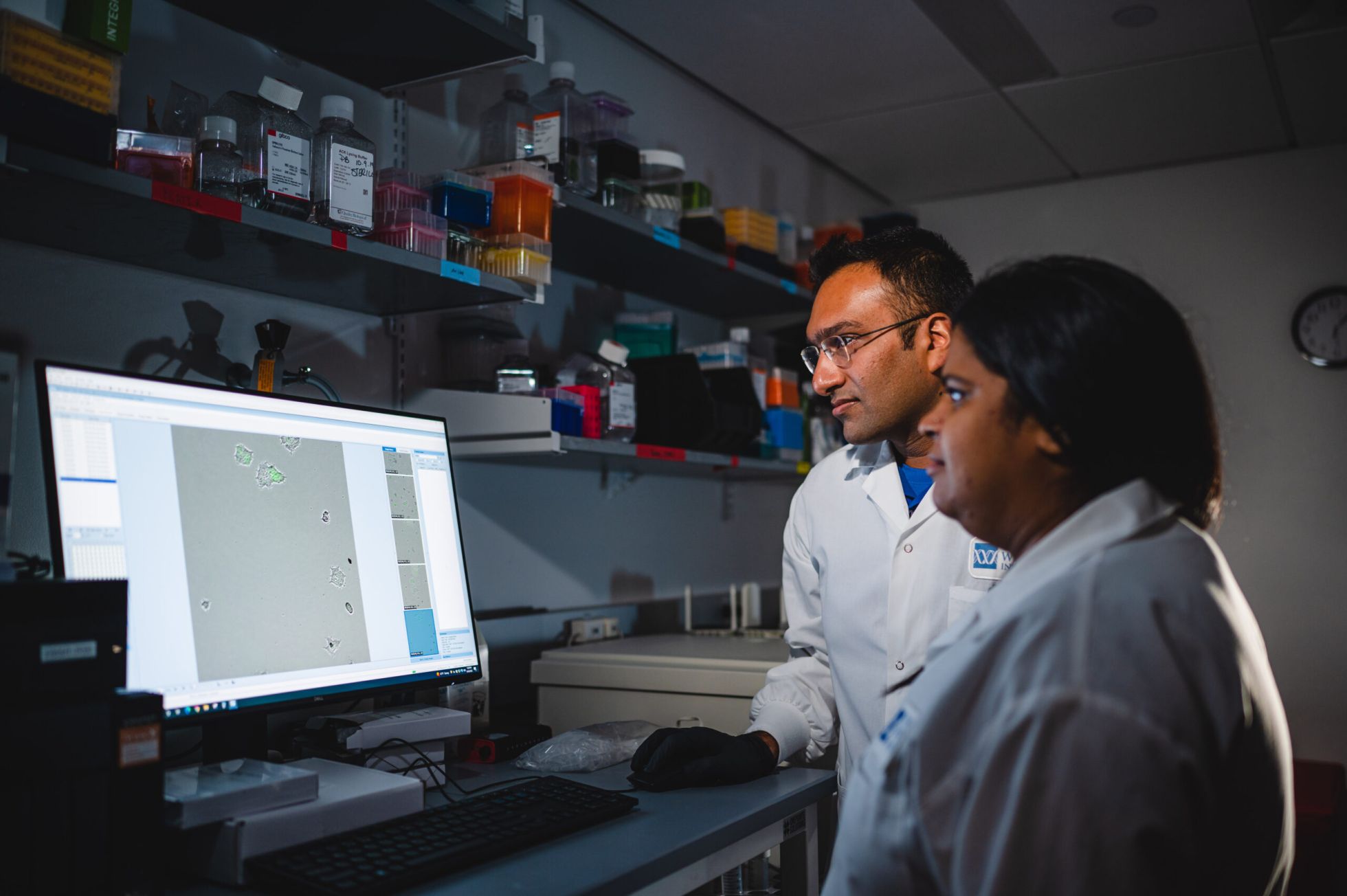
Accelerating Discovery
Wistar Scientists are Making Discoveries that Improve Human Health
Wistar Science
Want to stay up-to-date with Wistar Science? Click here.
Donate
Ensure Wistar researchers have the freedom to pursue new ideas to make the greatest difference for humankind.
2024 Year in Review
Together, we empower the potential, promise and impact of Wistar Science.


