The Wistar Institute
Wistar Scientists Identify Pro-aging ‘Sugar Signature’ in the Blood of People Living with HIV
PHILADELPHIA — (April 10, 2024) — The Wistar Institute’s associate professor Mohamed Abdel-Mohsen, Ph.D., along with his team and collaborators, has identified sugar abnormalities in the blood that may promote biological aging and inflammation in pe…
Early-Stage Discovery: How Wistar’s Genomics Facility Drives Wistar Science
Meet Sonali Majumdar, M.S., managing director of The Wistar Institute Genomics Facility, a hub that turns biological material into the data scientists need. Ms. Majumdar discussed the ins and outs of genomics technology and how Wistar Science depend…
Wistar Scientists Explore Importance of Microglia Marker in Metastasized Brain Tumor Microenvironment
PHILADELPHIA—(Mar. 28, 2024)— The Wistar Institute’s Qing Chen, M.D., Ph.D., assistant professor in the Immunology, Microenvironment and Metastasis Program at the Ellen and Ronald Caplan Cancer Center, has discovered certain immune cells in the brai…
Formulating a love for science
Kensington Health Sciences Academy students get hands-on experience and exposure to Wistar Science Standing in The Wistar Institute’s state-of-the-art training lab, a small group of 12 students gathered quietly around a large digital display project…
Wistar in the News: Inquirer story on new Wistar-PCOM Cancer Biology Ph.D. Program
The Wistar Institute was featured in The Philadelphia Inquirer for the launch its new Cancer Biology Ph.D. Program with Philadelphia College of Osteopathic Medicine. Reporter Sarah Gantz detailed how the jointly run Ph.D. program will offe…
PCOM, The Wistar Institute Announce Cancer Biology Graduate Program
Marking the next step in their innovative academic collaboration, Philadelphia College of Osteopathic Medicine (PCOM) and The Wistar Institute have announced the launch of a highly anticipated Cancer Biology Ph.D. Program aimed at advancing research…
Wistar Scientists Study What Cancer Cells Crave
Wistar’s Zachary Schug and lab are studying the relationship between alcohol intake and some site-specific cancers What do cancer cells need to thrive and grow? The Wistar Institute’s Zachary Schug, Ph.D. — assistant professor in the Molecular and C…
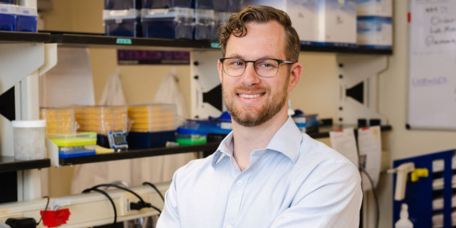
Dr. Dan Claiborne’s Discoveries That Catalyze New Discoveries
Daniel Claiborne, Ph.D., was recruited to The Wistar Institute through the Caspar Wistar Fellowship program, which fast-tracks promising early-career investigators to full faculty membership. Now an assistant professor in Wistar’s major research cen…
Wistar’s 2nd Annual Trainee Research Symposium Showcases Research Inspiration for Early Career Scientists
Wistar capped off its second-ever Trainee Research Symposium on Friday, February 23, drawing more than 200 research trainees of all levels from across the region and beyond. Next-gen student scientists, bringing interests spanning a range of researc…
Whether it’s a business opportunity or a flower bed, The Wistar Institute’s Kathy Day helps it flourish
We talked with Kathy Day, administrative coordinator for the Business Development and Legal departments, on her path to Wistar, what she loves about her work, and her passion for gardening. What does your day look like? I arrive at work very early –…