The Wistar Institute
“Science is the Answer” Celebrated at Wistar Party
In the beautiful setting of the College of Physicians of Philadelphia, Wistar friends attended this year’s Wistar Party, a celebration of Wistar science that has carried on for decades, and an opportunity for the Institute to express its gratitude t…
Enhanced Anticancer Compound May Allow for Precise Activation and Tracking of Treatment
PHILADELPHIA — (May 15, 2019) — Researchers at The Wistar Institute and the University of South Florida have advanced a novel compound that specifically targets the endoplasmic reticulum (ER) stress response that is frequently hyperactivated in canc…
A Tale of Families, Genes and Resilience
Recently, Wistar had the great honor of bestowing its annual Women & Science’s Helen Dean King Award upon Dr. Mary-Claire King, one of the most esteemed and productive scientists of our time, in recognition of her seminal contributions to scienc…
Wistar Joins in a Celebration of Science Education at the Philadelphia Science Festival
Along with warmer temperatures and the beautiful blossoming across the city, spring has become synonymous with the Philadelphia Science Festival, a staple and model for similar initiatives in other cities, that continues to grow each year. Establish…
How CURE Boosts the Health of Pennsylvanians
Each year in early May, representatives from Wistar and fellow institutions who are part of the Pennsylvania Cancer Alliance engage legislators to reinforce the importance and impact of CURE funding. The Commonwealth Universal Research Enhancement P…
Wistar Earns ‘Exceptional’ Rating for NCI Cancer Center Support Grant for the Second Review Cycle in a Row, Demonstrating Strength of Science
PHILADELPHIA — (April 23, 2019) — After extensive peer review, The Wistar Institute’s Cancer Center has received an “exceptional” rating on its Cancer Center Support Grant (CCSG) application from the National Cancer Institute (NCI) for the second re…
Wistar Science Highlights: Zika Infection, Cancer Immunology and Immunotherapy
In a study published online in Nature, the lab of Dmitry I. Gabrilovich, M.D., Ph.D., Christopher M. Davis Professor and leader of the Immunology, Microenvironment and Metastasis Program, identified a critical step that happens when parts of the imm…
Signed, Sealed and Credentialed: Biomedical Technician Training Program is an Accredited Pre-apprenticeship Program in the Commonwealth of PA
For two decades, Wistar’s Biomedical Technician Training (BTT) pre-apprenticeship program has injected biomedical talent into the region’s life sciences workforce by ushering class after class of promising Community College of Philadelphia (CCP) stu…
Innovative Synthetic DNA-based Cancer Immunotherapy Approach Shows Tumor-clearing Ability in Preclinical Models
PHILADELPHIA — (April 18, 2019) — Wistar scientists have developed a novel synthetic DNA approach for patient-specific production of cancer-targeting molecules called bispecific T cell engagers. DNA-encoded bispecific T cell engagers (dBiTEs) design…
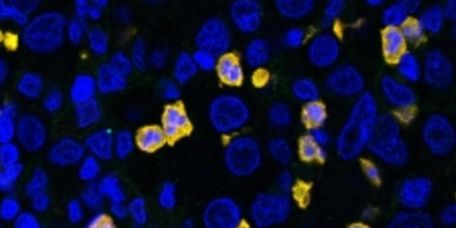
Identification of a Critical Regulator of Immune Suppressive Cells Reveals a Novel Target for Cancer Immunotherapy
PHILADELPHIA — (April 17, 2019) — Wistar scientists have identified a critical regulator of the function of myeloid derived suppressive cells (MDSCs), opening new opportunities for specific therapeutic targeting of these cells to inhibit tumor growt…