The Wistar Institute
New Insights Into the Control of Inflammation
PHILADELPHIA — (Jan. 13, 2021) — Scientists at The Wistar Institute discovered that Early Growth Response 1 (EGR1), a protein that turns on and off specific genes during blood cell development, inhibits expression of pro-inflammatory genes in macrop…
Wistar Researchers Develop New Humanized Mouse Model That Provides Insight Into Immunotherapy Resistance
PHILADELPHIA — (Jan. 12, 2021) — Scientists at The Wistar Institute have created an advanced humanized immune system mouse model that allows them to examine resistance to immune checkpoint blockade therapies in melanoma. It has revealed a central ro…
Wistar Scientists Target an Alternative Fuel Source of Cancer Cells as a Therapeutic Approach for Breast Cancer
PHILADELPHIA — (Jan. 7, 2021) — Scientists at The Wistar Institute characterized an inhibitor that targets acetate metabolism in cancer cells. Cancer cells use acetate metabolism to support tumor growth in conditions of low nutrient and oxygen avail…
The Wistar Institute and Batavia Biosciences Launch Collaboration to Manufacture and Distribute Wistar’s Rubella Vaccine Globally
PHILADELPHIA — (April 29, 2020) — The Wistar Institute and Batavia Biosciences announce the launch of a strategic collaboration aimed to streamline the clinical grade manufacture and global distribution of Wistar’s rubella vaccine seed stock commonl…
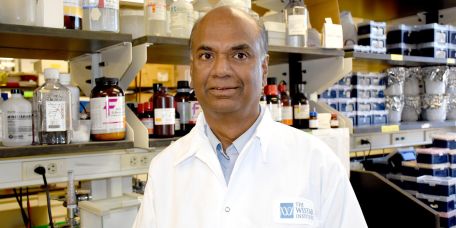
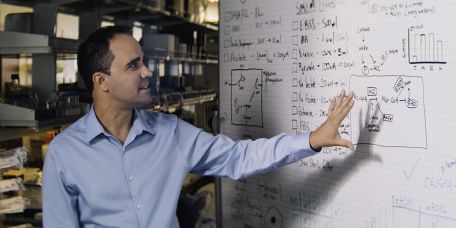
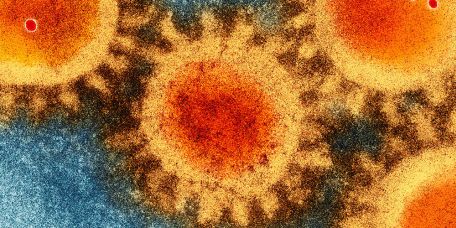
Spotlight on Wistar COVID-19 Researchers: Luis Montaner, D.V.M., D.Phil., & Joseph Salvino, Ph.D.
Dr. Luis Montaner is an HIV expert focused on finding new ways to boost the natural function of the immune system to combat infection or viral-associated disease. Dr. Joseph Salvino is a medicinal chemist and an expert in drug discovery and identifi…