The Wistar Institute
The Wistar Institute Announces COVID-19 Vaccine Mandate for All Employees
PHILADELPHIA — (June 2, 2021) — The Wistar Institute, an international biomedical research leader with special expertise in cancer, immunology and infectious disease research and vaccine development, will require all employees to be vaccinated again…
The Wistar Institute Recruits Noam Auslander, Ph.D., as Assistant Professor to Bring Artificial Intelligence Research to Its Cancer Center
PHILADELPHIA — (June 1, 2021) — The Wistar Institute, an international biomedical research leader in cancer, immunology and infectious diseases, announces the appointment of Noam Auslander, Ph.D., as assistant professor in the Molecular and Cellular…
Discovering the Mechanisms That Fine-tune Gene Expression
Turning on or off one or more genes at the wrong time or in the wrong cells can dramatically alter their activity and lead to unrestrained growth and cancer. Therefore, numerous control mechanisms are in place to keep the whole process in check…
The Wistar Institute and Other Top U.S. Cancer Centers Call for Urgent Action to Get Cancer-Preventing HPV Vaccination Back on Track
PHILADELPHIA – May 20, 2021 – The Wistar Institute has partnered with doctors and scientists across America at National Cancer Institute (NCI)-designated cancer centers to issue a joint statement urging the nation’s physicians, parents and young adu…
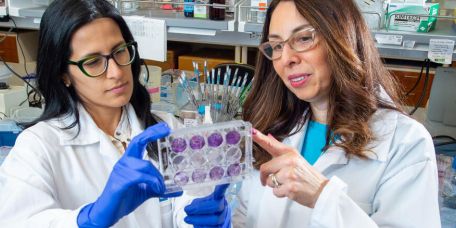
Celebrating 15 Years of Protecting Children’s Health Worldwide
Milestone discoveries made at The Wistar Institute have led to the development of vaccines that protect children and adults from widespread and life-threatening diseases and have saved countless lives in the United States and around the world.&…
May is National Cancer Research Month
Wistar joins the American Association for Cancer Research and many other organizations in raising awareness on the importance of cancer research. In 2018, the world saw more than 18 million new cases and 9.5 million cancer-related deaths*. Research…
Groundbreaking of Life Science Building Encapsulates West Philadelphia Growth and Power of Partnership
University Place Associates (UPA) celebrated the groundbreaking of soon-to-be-constructed 3.0 University Place, a more than 250,000 square foot, technologically advanced and environmentally sustainable life science building in West Philadelphia that…
Wistar and Peter Mac Scientists Discover Fundamental Mechanism That Fine-tunes Gene Expression and Is Disrupted in Cancer
PHILADELPHIA and MELBOURNE, Australia — (May. 17, 2021) — A team of scientists from The Wistar Institute in Philadelphia and the Peter MacCallum Cancer Center in Melbourne, Australia, discovered a new checkpoint mechanism that fine-tunes gene transc…
Wistar Expands International Training of the Next Generation of Scientists With the University of Bologna
PHILADELPHIA — (April 27, 2021) — The Wistar Institute and the University of Bologna (Unibo) in Italy have established the Wistar-Unibo Ph.D. Exchange Program in Cell and Molecular Biology to bring Unibo graduate students to Wistar for their three-y…
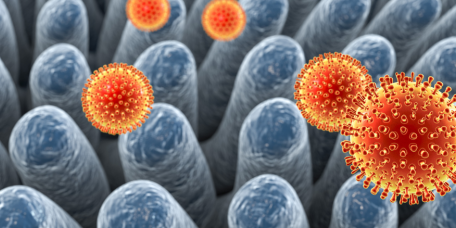
Latest Wistar Discoveries: Fine-tuning Vaccine Delivery in Preclinical Models to Advance MERS DNA Vaccine Candidate and Discovering New Targets for Cancer Therapy
A team of Wistar scientists led by Dr. David Weiner, Wistar executive vice president, director of the Vaccine & Immunotherapy Center and W.W. Smith Charitable Trust Professor in Cancer Research, and Dr. Ami Pat…