The Wistar Institute
The Wistar Institute’s Head of HIV Cure and Viral Diseases Center Luis Montaner Shares Why He Thinks We Can Attain an HIV Cure
Finding a cure has long been the holy grail of HIV research. Now new discoveries are putting that goal within reach, according to Wistar’s Luis Montaner, D.V.M., D.Phil.
As director of the institute’s new HIV Cure and Viral Diseases Center, Montane…
Newsweek Magazine in Collaboration with Best Practice Institute Recognizes The Wistar Institute in 2025 ‘Excellence Index’
PHILADELPHIA — (December 20th, 2024) — In its annual Excellence Index, Newsweek and the Best Practice Institute has recognized The Wistar Institute as one of the world’s top 1000 companies. Wistar led the way as the top-ranked company in the Healthc…
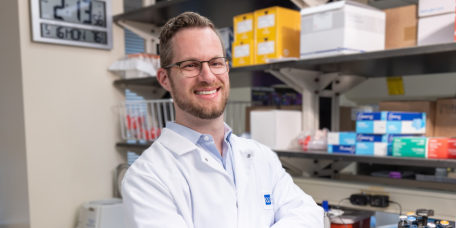
How The Wistar Institute’s Dr. Dan Claiborne Engineers CAR T Cells to Fight HIV
Assistant professor Daniel Claiborne, Ph.D., pursues one of the hottest up-and-coming areas of research: CAR T cells, which are engineered immune cells designed to attack specific target Dr. Claiborne’s work focuses on HIV. As Dr. Claiborne prepares…
The Wistar Institute Receives Two Biomedical Research Grants from the V Foundation for Cancer Research
PHILADELPHIA — (December 10, 2024) — The Wistar Institute assistant professors Nan Zhang, Ph.D., and Noam Auslander Ph.D., have both received independent funding totaling $1.2 million over the next three years for cancer research projects from the V…
Wistar Institute Researchers Design Novel Immunotherapy for Brain Cancer
PHILADELPHIA — (December 3rd, 2024) — The Wistar Institute’s David B. Weiner, Ph.D. — Executive Vice President, director of the Vaccine & Immunotherapy Center and W.W. Smith Charitable Trust Distinguished Professor in Cancer Research — and his lab h…
The Wistar Institute Awarded $2 Million RACP Grant from Shapiro Administration for New Center for Advanced Therapeutics
PHILADELPHIA — (Nov. 27, 2024) — Governor Josh Shapiro’s Administration, through the Commonwealth of Pennsylvania Redevelopment Assistance Capital Program (RACP), has granted The Wistar Institute $2 million to fund its new Center for Advanced Therap…
Trailblazing Nobel Laureate Dr. Katalin Karikó Meets with Wistar Trainees
Dr. Katalin Karikó, 2023 Nobel Laureate in Physiology or Medicine, received The Wistar Institute’s 2024 Helen Dean King Award and as a part of the day-long activities, Dr. Karikó spent time with Wistar trainees listening, answering their questions a…
The Wistar Institute’s Dr. Rahul Shinde Shares Hopes for Future of Pancreatic Cancer Therapy
For Pancreatic Cancer Awareness Month, we sat down with Rahul S. Shinde, D.V.M., Ph.D., assistant professor in Wistar’s Ellen and Ronald Caplan Cancer Center who researches potential new therapies for treatment-resistant cancers like pancreatic canc…
Wistar Institute Researchers Discover New Combination Therapy Approach for Metastatic Ovarian Cancer
PHILADELPHIA — (November 21, 2024) — The Wistar Institute’s Nan Zhang, Ph.D., assistant professor in the Ellen and Ronald Caplan Cancer Center’s Molecular and Cellular Oncogenesis Program, and lab have discovered a new approach to treating ovarian c…
Collaboration between The Wistar Institute and Cameroon Researchers Reveals HIV Latency Reversing Properties in African Plant
PHILADELPHIA — (November 19, 2024) — A collaboration between The Wistar Institute and the University of Buea in Cameroon has uncovered the mechanisms for a medicinal plant with anti-HIV potential in Croton oligandrus Pierre & Hutch, a species of Afr…