The Wistar Institute
Global Voices for HIV Advocacy and Cure Research Come Together at Wistar’s 26th Annual Jonathan Lax Lecture
This year, The Wistar Institute hosted the Annual Jonathan Lax Memorial Award Lecture virtually, bringing together HIV scientists and activists on a global stage. Celebrating 26 years of continuous HIV research collaboration, the event was streamed…
Taking on Cancer
Philadelphia Business Journal senior health reporter John George hosted Taking on Cancer, a two-panel discussion that kicked off with perspectives from local research leaders at the helm of world-class research institutes and health care systems. It…
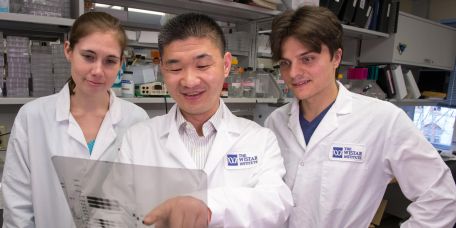
Wistar Scientists Identify Novel Therapeutic Approach to Re-activate Immune Response Against Tumors
PHILADELPHIA — (June 21, 2022) — Due to the development of resistance to chemotherapy and recurring tumors, patients with ovarian cancer often have low survival rates. Therefore, new therapeutic options such as targeted therapy that boosts anti-tumo…
Wistar’s Dr. Amelia Escolano Named 2022 Pew Scholar
PHILADELPHIA — (JUNE 14, 2022) — The National Advisory Committee of the Pew Scholars Program in the Biomedical Sciences, has chosen Amelia Escolano, Ph.D., Assistant Professor in The Wistar Institute’s Vaccine & Immunotherapy Center, to join the…
Pennsylvania Department of Labor and Industry and Legislator Tour Wistar
The Wistar Institute was awarded a PAsmart grant of $650,000 from the Pennsylvania Department of Labor & Industry to expand education and training programs further across the region and create additional opportunities for more students to prepar…
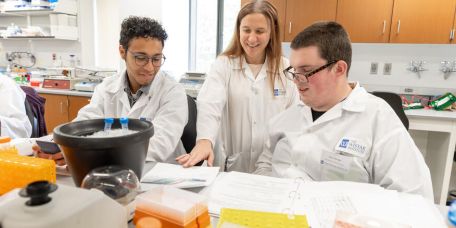
Wistar Grows its Collaborative Network Offering Internships in Biotechnology and Life Sciences
Wistar’s Biomedical Technician Training (BTT) Program was developed with the commitment to provide its students hands-on training and industry experience not traditionally delivered in academic classrooms. The Wistar Institute’s training program has…
Wistar Science Synergy Through Fostering International Collaborations
Inaugural graduate students from Leiden University Medical Center speak to their Wistar experience. The Wistar-Schoemaker International Postdoctoral Fellowship is a special exchange of postdoctoral fellows between our two institutes. We sat down wit…
Discussing the Mysteries of Melanoma
A Q&A with Drs. Chengyu Liang and Meenhard Herlyn on skin cancer research at The Wistar Institute, including a few questions from melanoma survivors. Melanoma is the most aggressive form of skin cancer. Work at The Wistar Institute’s Melanoma Re…
Spotlighting Wistar’s Cheyney University Student Scientists
Read some reflections from the Cheyney University students who participated in Wistar’s Biomedical Research Methods course during Spring 2022. Lights, lab coats, action! The click of pipettes and low murmur of voices fill the open lab space as stude…
Wistar’s Shark Tank Pitch Competition Goes Swimmingly
The hybrid event marked the conclusion of the Institute’s Life Science Innovation Course that provides experience in biotechnology entrepreneurship. Students enrolled in The Wistar Institute’s Life Science Innovation course entered the shark ta…