The Wistar Institute
Wistar Scientists Successfully Engineer a Goldilocks Construct: Therapeutic Antibody Could Be a Future Medicine to Improve Outcomes for Melanoma
In recent years, multimodal therapies have emerged as a route to treat cancer by delivering different types of treatments together to improve effectiveness. However, the more modalities there are, the more complex the production and effects of these…
Balancing Act: It’s a Fine Line Between Inflammation and Immunity When Viruses are Involved
Dr. Mohamed Abdel-Mohsen’s Pioneering Research on Siglecs Spotlights Their Role Helping the Immune System Recognize Viral Infections, and as Promising Future Therapy Dr. Mohamed Abdel-Mohsen and his virology lab at The Wistar Institute review t…
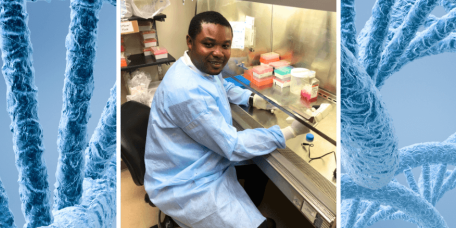
Coordination/Synthetic Chemist Returns to Cameroon Ready to Train Next Generation of African Scientists on Wistar’s World-Class Analytic Chemistry Techniques
“Our hope is to build a center with the same reflection of Wistar in science and administration.” In three short months as a Visiting Scholar with The Wistar Institute in Philadelphia, Donatus Bekindaka Eni, BSc., MSc., Ph.D., a lecturer from the Un…
Notes From the Field: Seeing Research in Action
More than 1,000 supporters gathered in Fairmont Park for PanCAN PurpleStride Philadelphia 2023 to support the Pancreatic Cancer Action Network (PanCAN). Wistar’s Dr. Rahul Shinde is a PanCAN research grant recipient, and our lab was honored to atten…
After 10 Years as Chief Financial Officer, Joe Trainor Readies for Retirement
It is often said that the measure of a person is in more than just their accomplishments. For Dario Altieri, CEO of The Wistar Institute, trying to sum up the tenure of Joe Trainor, who will be retiring this month as Wistar’s Chief Financial Officer…
GeneOne and Wistar Institute Collaborate to Develop Small Molecule Therapeutics to Protect Humans from Nipah Virus
PHILADELPHIA — (May 10, 2023) — GeneOne Life Science, Inc.(“GeneOne” KOSPI: 011000), a leading biopharmaceutical company specializing in developing nucleic-acid based treatments and novel small-molecule therapeutics, and The Wistar Institute, an int…
The Wistar Institute, Pennsylvania Biotechnology Center and Baruch S. Blumberg Institute Forge Strategic Collaboration to Support Regional Biotech Startups
PHILADELPHIA — (MAY 9, 2023) — The Wistar Institute has formed a new strategic collaboration with the Pennsylvania Biotechnology Center (PABC) and the Baruch S. Blumberg Institute to accelerate the advancement of “bench to bedside” biomedical resear…
Wistar Scientists Discover Innate Tumor Suppression Mechanism
PHILADELPHIA — (MAY 4, 2023) — The p53 gene is one of the most important in the human genome: the only role of the p53 protein that this gene encodes is to sense when a tumor is forming and to kill it. While the gene was discovered more than four de…
Second Annual Shark Tank Event is Smooth Sailing for Students
Students participating in the Institute’s Life Science Innovation Course cap their experience with a final business pitch. Over a cup of coffee several years ago, Dr. David Zuzga, Associate Dean of Biomedical Studies, and Heather Steinman, Senior VP…
Dr. Luis Montaner Visits Vietnam for Official Launch of AMOHI Clinical Trial
Montaner, together with international delegations, attended the April 4 launch in Ho Chi Min City. On April 4, tucked in a courtyard at the Go Vap District Health Center in Vietnam’s Ho Chi Min City, Dr. Luis J. Montaner joined local and internation…