Melanoma Researchers Gathered at Wistar to Discuss Disease Progression and Therapy Resistance
Dedicated to the memory of melanoma research champions Dr. Shyam Somasundaram, Wistar scientist, and Eleanor Murdoch, melanoma advocate and mother of Noreen and Kate O’Neill, this year’s Symposium brought together international experts in basic and translational research to share their latest advances to understand disease progression and therapy resistance.
Both targeted therapies and immunotherapy have brought transformative improvements for melanoma treatment, increasing the average life expectancy for some patients with advanced disease from a matter of months to a matter years.
“Despite the substantial advances, we’ve reached a plateau in our ability to overcome therapy resistance and further improve patient survival,” said Dr. Keith Flaherty, director of Clinical Research at the Massachusetts General Hospital Cancer Center.
Researchers are focused on addressing resistance as a way to increase the fraction of patients who respond to these therapies and to fight tumors that come back after an initial response.
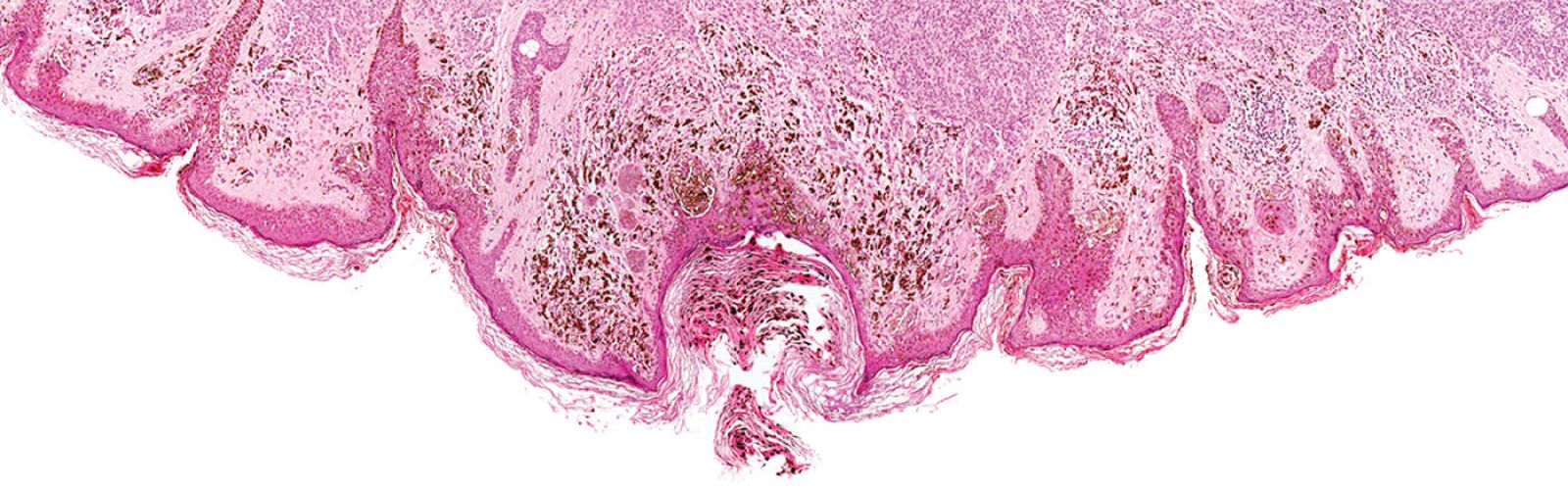
Targeted therapies work by blocking specific molecular targets that support the growth, progression, and spread of cancer. Scientists have identified two major ways melanoma cells evade these therapies. One involves reactivating the specific mechanism that is being blocked, for example by making more gene copies to produce more of a certain protein. Another trick is for cells to change their identity by switching on and off a set of genes that define their functions and behavior, so that they no longer need the protein targeted by the therapy.
New approaches aim to find vulnerabilities that can be exploited to kill melanoma cells after they’ve re-programmed themselves to resist therapy.
Dr. Thomas Graeber, professor and director of the Metabolomics Center at the University of California, Los Angeles, is studying drugs that cause a unique type of iron-dependent cell death called ferroptosis as a tool to enhance response to targeted therapies and immunotherapy.
Success of immunotherapy depends on the ability of our immune system to recognize and react to proteins that are specifically produced by melanoma cells as a result of genetic mutations and other mechanisms. These proteins, known as neoantigens, are critical because they flag tumor cells as dangerous or unwanted. Dr. Yardena Samuels, associate professor of Molecular & Cell Biology and the Knell Family Professor at the Weizmann Institute of Science in Israel, is applying high-throughput approaches to identify neoantigens that could be used to create cancer vaccines and other immunotherapies.
Epidemiologist Marianne Berwick, distinguished professor and associate director of Cancer Population Sciences at the University of New Mexico, leads an international team of investigators who have built a large collection of melanoma samples from patients in the U.S., Australia and Spain to identify new biomarkers that can inform better therapeutic approaches.
Melanomas are naturally heterogeneous tumors, with different subpopulations of cells that differ in aggressiveness and response to therapy. This heterogeneity is observed between patients and even within the same patient and represents an obstacle for immunotherapy success.
Medical oncologist Jedd Wolchok, chief of the Melanoma and Immunotherapeutics Service and the Lloyd J. Old Chair for Clinical Investigation at Memorial Sloan Kettering Cancer Center, and his team are investigating ways to potentiate immunotherapy approaches to overcome heterogeneity and kill resistant cells.
Dr. Wolchok has been at the forefront of cancer immunotherapy both as a research scientist exploring innovative strategies in laboratory models and as a principal investigator in many pivotal clinical trials. He recently led a global phase 3 trial to identify the most effective combination checkpoint blockade therapy for melanoma, which had a 58% response rate.
“We’ve reached an average survival of 72.1 months, which is a huge improvement compared to what we could do before immunotherapy and targeted therapy,” said Dr. Wolchok. “But immunotherapy doesn’t work for everybody, and has a high frequency of toxicity, so we still have work to do to sharpen the risk/benefit ratio and help the nearly half of patients who don’t benefit from this combination therapy.”
He thinks that some patients might need an additional boost with different types of immunotherapy. His lab is studying engineered T cells that are modified in the lab to attack melanoma cells presenting a certain protein. They have found that these T cells can also kill tumor populations that don’t express that same antigen, an effect called bystander tumor killing, with the help of other immune cells called neutrophils.
In closing the event, Dr. Jessie Villanueva, associate professor at The Wistar Institute Cancer Center who leads a productive research team working on therapy resistance and hard-to-treat melanomas, invited everyone back for the fifth edition.
All the speakers look forward to next year’s Symposium to be held in person at the Institute.